Frequency and associated factors of mental health disorders among healthcare workers in developing and developed countries.
Abstract
This chapter gives an insight into the psychological journey of the essential healthcare workers (HCWs) during the COVID-19 pandemic. The catastrophe which started off with uncertainty, provoked fear-related behaviors among the frontline doctors, nurses and paramedical staff. With meager resources and lack of a disaster plan, fire-fighting was a reflex response of healthcare institutions. Though the whole world seemed to be unprepared for the calamity, developing countries with fragile healthcare systems were more vulnerable to collapse. The negative aura was complicated by mistrust among the general population, regarding healthcare workers, institutions and government. Furthermore, with economic downfall; balancing work and protecting the family was a challenge for HCWs, especially during the pandemic peak. The psychological distress translated to rising incidence of depression and anxiety among them. As institutions gained insight into psychosocial issues of HCWs; support and therapies were offered to them. Positive messages labelling HCWs as “Heroes of the Pandemic” were circulated and structured programs developed to address their needs. With the advent of COVID-19 vaccine, a ray of hope emerged, although there are still apprehensions about its efficacy and side-effects. The whole world now eagerly awaits the calamity to perish while normality can rise from ashes.
Keywords
- Health care worker
- Covid 19 Pandemic
- Anxiety
- Depression
- Phycological distress
1. Introduction
“2020” has been a revolutionary year especially in terms of exploring new healthcare horizons. The voyage of the pandemic which started off with crises, disbelief, qualms and fears; with the advent of the vaccine, seems to be ending with revival, hope, insights and new acumens.
In its true sense, within a couple of months the world transformed into a global village attacked by a common enemy “The SARS COVID-19 virus” with healthcare workers (HCW) stepping into the battlefield, leading from front; few losing their lives while the others still struggling to get through the catastrophe. Although the unsung heroes are working nonstop under tremendous pressure, surely the effects of this struggle may take a long time to fade. Especially the psychological pressure, stress and burnout may leave long lasting effects such as post-traumatic stress disorder, anxiety and depression which may continue to shape their lives in the long term.
This chapter gives an insight into the psychological journey of the essential healthcare workers; doctors, nurses and paramedical staff who are selflessly working at the frontlines, caring for their patients while striving to protect themselves, their families and loved ones from the outbreak. The chapter discusses the psychological distress caused, its associated factors and the coping strategies developed. As the pandemic is still not over, with the long term efficacy of vaccine unknown and as the third wave is approaching, recommendations can be made for preventive measures to limit the damage.
2. The beginning - Fear of unknown
The infection was first reported as a case series of patients with pneumonia in Wuhan, China in December 2019. Tracing back exposure, all the cases were found to have visited a seafood market in Wuhan. The virus identified as a new strain of Corona virus, was later named as COVID-19 [1]. More than 200 countries and around 500,000 population worldwide were affected within a short span on 3–4 months, while death attributable to COVID-19 globally was reaching more than 20,000 by the end of March 2020 [2]. Though the whole world seemed to be unprepared for the calamity, developing countries with fragile healthcare systems were more vulnerable to collapse [3]. With a mortality rate as high as 12% reported in industrialized countries, the general speculations were devastating [4, 5].
2.1 Fear of disease and shortage of Personal Protective equipment
Soon, the xenophobia spread to communities, institutions, regional and international governance while all the hopes to address, control and prevent widespread damage from the infection were laid on scientists, public health and medical professionals. High expectations from healthcare workers (HCWs) who were themselves vulnerable and exposed, further complicated the situation especially in an overwhelming situation with resource constraints. Healthcare workers including front line physicians, nurses and paramedical staff combating at forefront were especially susceptible to get infected, taking the disease back home and infecting their family members. As the association of higher mortality with older age became evident, the senior health professionals and their families were even more concerned for the health of their loved ones [6, 7].
Due to unpreparedness, availability of personal protective equipment (PPE) was limited even for the healthcare professionals, let alone for the general population. Dearth of knowledge about nature of disease and its spread, further created mental pressure and psychological distress [3]. Institutions which were already overburdened and functioning beyond their limits, were unable to provide adequate support to the petrified HCWs.
2.2 Psychological distress and associated factors
The beginning of the pandemic was therefore taxing for the mental wellbeing especially of healthcare professionals. Various studies among frontline physicians, nurses, para medical and administrative staff, revealed a high prevalence of stress, anxiety and depression [8] as depicted in Table 1. Although most of the studies did not compare the prevalence of mental distress during COVID than the pre-COVID era, but generally there was an alarming frequency of stress, anxiety and depression during the pandemic [25]. A study found a higher likelihood of anxiety, depression and lower quality of life scores among HCWs involved in COVID response than those who worked in other areas [26]. Another study in Italy revealed that healthcare professionals who were working with COVID patients were twice as likely to seek psychological help during the pandemic, than those working in other areas [27].
| Healthcare worker | Subjects | Country | Frequency | Associated factors/ predictors of depression/anxiety | |
|---|---|---|---|---|---|
| Developing countries | |||||
| [3] Physicians | 389 | Pakistan | 43% physicians had depression |
| |
| [6] HCW (Majority nurses) | 365 | Jordan | High fear score 40% extremely severe depression, 60% extremely severe anxiety 35% severely distressed |
| |
| [9] Doctors, nurses and paramedics | 476 | South Asian countries | 25.7% prevalence of depression |
| |
| [10] HCW | 908 | China | 16.63% moderate/severe anxiety 18.29%moderate/severe depression 24.50% concomitant moderate/severe anxiety and depression |
|
|
| [11] HCWs (doctors, health assistants, auxiliary nurse-midwifery, nursing students posted in the wards, laboratory assistants, paramedics, staff nurses, sanitization workers, ward attendants, security guards and ambulance drivers) | 150 | Nepal | Prevalence of anxiety disorder was 37.3 %, 8% of the participants had depression Overall, 38 % of the participants, had at least one psychiatric illness | - | |
| [12] Frontline medical imaging staff | 5331 | China | Frequency of anxiety disorders were 6.5% and higher than those of anxiety and depression in Chinese residents before the epidemic. | - | |
| [13] Healthcare workers | 331 | Cameroon | Anxiety (41.8%) and depression (42.8%) |
| |
| HCWs [14] | 433 | India | High-level stress in 3.7% Depressive symptoms requiring treatment and anxiety symptoms requiring further evaluation were 11.4% and 17.7% respectively |
| |
| [15] HCWs | 1146 | India, Indonesia, Singapore, Malaysia and Vietnam | 4.5% screened positive for depression, 5.2% for anxiety India had the lowest prevalence of depression 0.8%, Indonesia 2.4% Singapore 4.7%, Vietnam 6.7% and Malaysia (14.3%). |
| |
| [7] HCWs | 745 | Libya | 56.3% participants had depressive symptoms 46.7% had anxiety symptoms |
|
|
| [16] Nurses | 2,014 | Wuhan, China | 14.3%, 10.7% and 91.2% nurses reported moderate to high levels of anxiety, depression, and fear | Mental health outcomes negatively correlated with
| |
| [17] Frontline nurses | 325 | Philippines | 37.8% were found to have dysfunctional levels of anxiety |
| |
| [18] Frontline nurses | 176 | Wuhan China | Mild, moderate and severe anxiety symptoms were found in 27.3%, 25%, and 25% |
| |
| [19] Nurses | 441 | Iran | 40% had moderate to severe anxiety. |
| |
| [20] Frontline nurses | 643 | Wuhan China | One-third (33.4%) reported anxiety | perceived stress and insomnia | |
| [21] Nurses | 3,228 | Sichuan Province and Wuhan City | 47.1% depression |
| |
| [22] Nurses | 586 | Eastern China | Frequency of anxiety and depression was 27.6% and 32.8%, respectively |
| |
| [9] HCWs (majority Physicians) | 939 | Turkey | 77.6% reported depression 60.2% anxiety 50.4% had insomnia 76.4% distress symptoms |
| |
| [10] healthcare workers | 218 | Italy | Prevalence of moderate to extremely severe symptoms in 8% for depression, 9.8% for anxiety, and 8.9% for stress. | Contributions of enhancement and suppression abilities and sensitivity to stressor context cues in predicting depression, anxiety determined. | |
| [11] HCWs (hospital, midwifery and administrative staff) | 600 | Dublin, Ireland | 20.3% of HCWs had moderate to severe depression and 21.0% had moderate to severe anxiety. 37% felt limitation of activity contributed to psychological deterioration. Household tensions were reported by 14% with partners and 20% with other household members including children |
| |
| [23] Neurosurgeons | 375 | 52 countries | 34% felt tense, 32.5 % unhappy and 14% had depression |
| |
| [12] Nurses | 255 | UK | 21% moderate to severe or severe anxiety depression (17.2%,) 18.9% had a low or very low resilience score. | Younger nurses with less experience have higher levels of anxiety and depression and had lower resilience. | |
| [13] Nurses | 1,005 | Italy | Prevalence of sleep disturbances, moderate anxiety and low self-efficacy was 71.4%, 33.23% and 50.65%, respectively | Females were more prone to sleep disturbances, anxiety and had lower levels of self-efficacy than male | |
| [24] Nurses | 270 | Turkey | 85.6% had high anxiety levels | Area of work in COVID ICU and perception of insufficient income was associated with anxiety | |
Table 1.
2.3 Stigmatization
As the infection built up its momentum and an epidemic transformed into a pandemic; there was an uneasiness among the medical professionals and other stakeholders. Fear of infection; especially spreading it to family members, long shifts in sub-optimal condition, lack of training and confidence created a vicious cycle of mistrust and negative professional attitude among physicians and nurses [28]. For example a study from china showed that mental health problems were more likely among nurses who regretted being in the field during the pandemic [29]. Another systematic review and meta-analysis showed high prevalence of anxiety and depression especially among female nurses [25].
Use of personal protective equipment (PPEs) by general population lead to an acute shortage and unavailability of masks and other PPEs for healthcare professionals, further complicating the situation. A lot of myths and false information were spread not only among the lay people but also the HCWs who were relying on news and social media for updates due to paucity of scientific data on the disease [3]. Stigmatization was therefore another factor associated with psychological distress and anxiety among HCWs [7]. In a nutshell, during the upsurge of the calamity, vulnerability to psychological distress was multifactorial and inevitable.
3. The Pandemic unfolding
3.1 Disaster plans
As the infection rapidly spread, the governments and health authorities experimented on various ways to contain and minimize spread of infection. Strict lock-downs were imposed and travel restricted, while standard operating procedures (SOPs) were formulated and implemented for essential services. Healthcare institutions and hospitals had to quickly devise a disaster plan, which included introducing secluded COVID clinics, emergency services, wards, high dependency units and intensive care units. Medical education came to a halt and post-graduate training was interrupted by special duties of medical and nursing trainees in COVID areas [30]. Other specialty doctors, nurses and paramedics were also trained to cover duties in COVID designated areas, as priorities shifted from non-emergency services to urgent care [23]. Elective surgeries and procedures were postponed and regular patient follow ups were deferred. On one hand this reduced the work load of healthcare workers offering services which were down the priority list; but physicians, nurses and paramedics on daily wages and incentives suffered financially. Private primary healthcare set-ups were closed to avoid unnecessary exposure of healthcare staff to infection while secondary and tertiary care hospitals dealt more with COVID and its associated emergencies. Follow up of patients with non-communicable diseases and elective surgeries were either deferred or the patients themselves opted to delay, due to fear of catching the virus. All procedures, laboratory work-up and diagnostic tests were also postponed, if risk of infection outweighed the benefits. Therefore, all the healthcare professionals offering non-essential services during the pandemic suffered financially.
This was indeed further taxing for HCWs working in private organization especially in developing countries, where insurance coverage and assistance from the government is minimal and often absent. Private institutions on the other hand were unable to cope up with the dipping revenue, which resulted in employers reducing salaries and forcing HCWs to take unpaid leaves [31].
3.2 Dealing with economic impact
The economic impact was generic for all other professions, in fact the intensity was even more for other professionals, with complete lock-downs, social isolation and closure of non-essential services. Therefore, the healthcare heroes had to fight back and make both ends meet with minimal support from other family members, especially during the initial surge of the pandemic. A study in Spain showed that frequency of suicidal ideation and behavior was high among COVID HCWs and the found to be associated with financial stress [32].
Moreover, in developing countries, unsatisfactory healthcare services even before the pandemic, provoked mistrust and apprehension among HCWs when they listened to horror stories from the media. The same was true for the best healthcare systems falling short to handle this overwhelming situation even in the developed world [33].
3.3 Rise of rate of infection among HCWs
With mistrust and economical pressure building up, the gravity of situation was further worsened by an exponential increased risk of infection among the healthcare workers. Physicians, nurses and para medics suffered with worst infections. By the mid of 2020, more than 1.5 million infections and 1400 deaths were reported among HCWs. Infections were more common among women and nurses while majority males and doctors died of it. General practitioners and mental health nurses were the highest risk specialties for deaths. For HCWs over 70 years of age the death rate was 37 deaths per 100 infections. The Eastern Mediterranean region had the highest number of reported deaths per 100 infections [34]. Besides risk of infection, the news of colleagues and acquaintances succumbing to it worked as a double edged sword, increasing psychological distress leading to stress, anxiety and depression among HCWs [23]. Furthermore, a feeling of helplessness and hopelessness prevailed when skilled medical experts were not able to help their patients to recover due to absence of available literature or clear scientific evidence on effective treatments; the phenomena of “moral injury”, as mentioned elsewhere in the chapter; The clinical guidelines issued by various regulatory bodies in a crises situation were weak and incomplete. Also there were a lot of discrepancies, making decision making further difficult for physicians, hence creating chaos and distress. The factors leading to mental disorders among HCWs during the pandemic therefore, were dynamic; creating a vicious cycle of increasing challenges, stress, inability to cope and more misery (Figure 1).
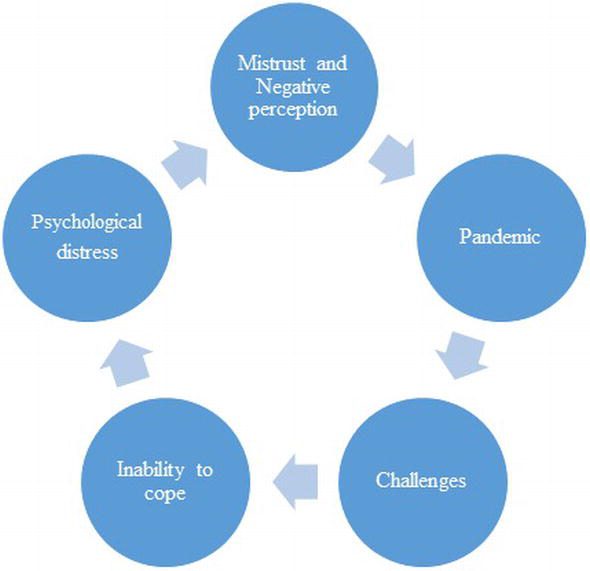
Figure 1.
Vicious cycle of psychological distress.
4. Reaching the peak of the curve
4.1 Impact on healthcare institutions
With the spread of infection, apprehension and fear was widespread among the general population. With an exponential increase in number of people getting infected, the panic was inevitable. This was especially evident in the developed countries, as the health systems though stable were not able to deal with the sudden surge of infected patients. While in the developing countries, an already fragile system with the overwhelming numbers reached to the verge of collapsing. As smaller scale healthcare set-ups were closed, tertiary care had to bear the brunt of all sorts of cases, from asymptomatic patients with anxiety to mild symptoms and severe symptoms, all reported in emergencies. This lead to overcrowding and hence compromising the quality of care. So much so that, a few private hospitals had to stop accepting new patients, due to unavailability of space in high dependency and intensive care units. This translated to a panic state among the general public. Hundreds of incidences of harassment and violence against healthcare workers were reported. Angry mobs went on to vandalize public and private properties on hospitals refusing to accept patients [35].
4.2 Misinformation and rumors
Misinformation and rumors spread all the wrong messages across non-medical people, further aggravating disbelief and mistrust. The “bad news” of the Pandemic was followed by a natural course of events. Initially, the public denied the presence of a new virus and labeled it as a “hoax perpetrated by a global cabal” and “a bio-weapon” [36]. Their illusions and imaginations went further wild when the healthcare authorities and professionals were unable to clarify their doubts with the little evidence and knowledge they themselves had about the disease. For example, initially it wasn’t clear if infected corpses were able to spread infection, so the staff were directed against handing over COVID infected corpses to relatives. This created doubts among the family already facing an emotional turmoil and rumors of political conspiracies spread, regarding hospitals tagging patients as “COVID infected” and retaining their dead bodies. Stigmatization against healthcare workers, COVID infected patients and medical infrastructure, therefore resulted in a high prevalence of violence, majority of which was directed against HCWs. Incidents of threats, physical and verbal assaults to the extent of HCW being shot were reported, especially in South-Asian and other developing countries [37]. The outcome was even worse with an already high frequency of burn out and psychosocial distress among HCWs [38]. With the healthcare system overburdened already at the peak of the pandemic, there was no time to for the government or healthcare authorities to respond to the hue and cries of HCWs.
4.3 Young and experienced HCWs affected
When little was known about complications of infection among elderly age group, the retired doctors were asked to help with managing the crisis, especially in UK [36]. As researches were conducted and it became evident that older age group was more likely to have grave complications and high mortality, a lot of senior and experienced physicians either chose to stay away or asked by their organizations to minimize exposure. Those who continued to work, felt even more distress with the risk of being exposed. On the other hand, younger HCWs feared taking the infection home to their elderly family members, hence a few studies also showed an association of young age with anxiety and depression among HCWs. This was especially prevalent in countries where a joint family system still prevails [21, 24]. The gravity of dissatisfaction among healthcare workers, especially nurses can be gauged by studies which revealed that not only nurses wanted to change their profession after the pandemic, but in Turkey, nursing students were found to be suffering from anxiety associated with a negative perception of their profession and an unwillingness to practice their profession in future [39].
4.4 Ethical dilemmas and distress
“Moral injury” is yet another form of psychological distress as a sequelae of actions, or the lack of them, which is against someone’s ethical code. This phenomena has been recently described in UK which is imposing a risk of psychological distress among HCWs, facing intense feelings of guilt due to the sub-optimal human resource and facilities available to deal with the suffering patients [40].
The overall situation was of resentment, hopelessness and dismay complicated by physical illness and rapid spread of infection among HCWs and their families, lead to an alarming frequency of mental health disorders like anxiety and depression among them.
5. From unknown to known- developing insight
Healthcare professionals are the main force on which foundation of healthcare system rests; hence eventually the government authorities and institutions realized the utmost importance of addressing their mental and physical wellbeing so that they can perform their duties in the most efficient manner. As the governments and healthcare authorities were able to consolidate their efforts, the need to address the psychological health of HCWs was felt. It was sensed that mental health of frontline healthcare workers required consideration, targeted prevention and intervention.
5.1 Interventions to support HCWs
Positive messages were spread across by regulatory bodies, local governments, national and multinational organizations at all platforms, labelling healthcare workers as “heroes of the pandemic”. Encouraging slogans like “Not all heroes wear capes, some wear scrubs” [41] were circulated in media, thanking HCWs for their efforts and for facing the predicaments from the front. Measures were taken to stop misinformation by circulating the correct information through visual, print and social from authentic sources like government, societies, NGOs and regulatory bodies (Figures 2 and 3).
Figure 2.
A message circulated by Centre of Disease Control (CDC).
Figure 3.
A message circulated by World Health Organization (WHO).
Protocols were made and zero tolerance policy was implemented by local governments to protect the HCWs from violence. For example India made violence against HCWs, a non-bail able offence with an imprisonment for 7 years, while Sudan created a special police task force to protect them. In June, the International Committee of Red cross in collaboration with World health organization (WHO) published a checklist for HCWs including managers, practitioners and policy makers for addressing the issue of violence against HCWs, which included procedures for risk assessment, response and accountability towards those receiving care [37].
Religious scholars also played a role in giving out the right information and convincing people for compliance with protocols. Moreover positive religious coping among HCWs was shown to be a negative predictor of anxiety and depression, so opening up of religious centers like mosques and churches after the peak subsided, may have promoted better mental health and psychological tranquility [42].
5.2 Psychological interventions
Similarly, regulatory bodies, health authorities, local and international governance and organizations are providing mental health support is through organized efforts to promote psychological wellbeing of physicians and nurses, and the outcomes have been shown to be encouraging. In Italy for example guidelines were implemented for providing frontline HCWs with psychological support and providing strategies for coping stress. Also surveillance programs to screen and follow HCWs for mental health were devised [40].
Work stress was shown to be a positive predictor of poor mental health [43]. Therefore, strategies to promote mental wellbeing, such as balanced diet and physical activity, stress relaxation and recreational activities, frequent breaks between work shifts, socializing and expressing emotions were promoted and shown to be effective in reducing anxiety and depressive symptoms among nurses [44]. A considerate and mindful leadership who is able to communicate, educate and support nurses to practice competently and safely (physically and mentally) in the context of COVID-19 was also shown to reduce anxiety and encourage resilience hence positively impacting their mental health [45]. Even online learning sessions on emotional freedom techniques sessions was shown to help improve mental health outcomes among nurses [46].
In Italy, a multidisciplinary team of psychologists and occupational therapists teamed up to provide frontline healthcare workers with psychological care based on coping strategies for managing stress [40].
The covid −19 pandemic started off with uncertainties and fear of unknown. With the excessive physical, social and psychological burden, especially on the lives of healthcare professionals, the fear gradually evolved to chronic anxiety. The focus in the current state should be to direct efforts to break this cycle as anxiety is just at the verge of transforming to hopelessness, anguish and depression. This is evident from the fact that while initially HCWs hoped the pandemic to end in a couple of months, after a year majority are uncertain as to how long the calamity would continue.
It is therefore imperative to intervene at this stage when the mental health of communities at large, especially HCWs is evolving from qualms to fear, anxiety and anguish which can be detrimental and challenging to reverse at a later stage, leaving them with post-traumatic stress disorder and hence low productivity.
5.3 Efforts generating better outcomes
As it is said, “For everything that divides, the human spirit unites”. As a result of these efforts, as compared to the general public while the frequency of anxiety and depression was high among HCWs before the peak, it descended after the peak [47]. A better insight into the disease its prevention and treatment could also have helped alleviate the anxiety among the physicians.
In a span of a year the situation came in a recovery phase with better insight, while just as SOPs were eased off and things seemed to be normalized, we were approached by the 2nd and 3rd surge of infection. Therefore, the hopes are now based on being able to target prevention through vaccines. It is speculated that with the advent of the vaccine, the social distancing protocols could be eased off. Moreover, a herd immunity as in the case of other deadly infections like small pox and polio, could eliminate the infection from the globe. This would normalize life as in the pre-COVID era and hence the distress would come back to baseline. From another perspective, if the vaccine is ineffective or if the innate ability of the virus to mutate quickly translates to a futile vaccine, the consequences may be unwarranted. Therefore, it’s too early to relax, as putting guards down can still lead to another deadly wave of infection, further causing more stress and trauma to the HCWs.
6. Rising from the ashes- A ray of hope
Nearly every accomplishment in this world is a result of a goal identified in a moment of crises or to fill a need. As the scientists worked tirelessly to gather more knowledge about the disease and its prevention, effective management and treatment guidelines were published. Physicians were able to work out prognosis and probabilities of complications, hence were able to offer better treatment modalities and patient care. The knowledge and confidence translated into a positive outlook and less distress among physicians. Finally, the news of near availability of effective vaccine was a sigh of relief for most HCWs.
6.1 Acceptability of vaccines and predictors
The uncertainty and qualms HCWs went through for more than a year was bound to inculcate doubts. Only 36% of the HCWs were sure to get the vaccine as soon as it was available, as shown by a survey in November 2020, with safety, efficacy and speed of development, “too good to be true” being major concerns [48] Other studies done to explore the readiness of HCWs to get vaccinated showed similar results, with senior HCWs more likely to take the vaccine immediately [49].
As education has been shown to be a predictor of vaccine uptake, it is more likely that in developing countries, the acceptability of vaccination would be lower than in developed nations. Yet, hopefully an insight into reduction in number of infected cases, hospital admissions and mortality will increase acceptability of the vaccine.
6.2 Way forward
Currently, the available vaccines have shown to be effective with minimal adverse effects [50] and HCWs all around the world have been given the first priority for vaccination followed by the most vulnerable; the geriatric age group. There is still some apprehension and doubts, even among HCWs about efficacy of different available vaccines, yet the overall impression is reassuring, especially, when one can anticipate the situation to gradually revert to normal. Moreover, with immunity to the infection, socialization without worrying for contacting an infection and traveling for the sake of leisure, professional and academic development can be made possible, with just an evidence of vaccination. Certainly the inflated incidence of mental health issues among the healthcare workers can be taken care of with the magic, a simple vaccine can create.
Although the year was tough especially on the HCWs adversity provokes fear related behaviors and affects the mental health negatively. Yet, it brings out the best in oneself, raising the probability of rising beyond the situation, promoting self-actualization, self-realization and resilience.
7. Conclusion
Healthcare workers quickly became the frontline force to help the world deal with the pandemic. The epidemic which quickly transformed into a pandemic, started off with widespread uncertainties and xenophobia, with HCWs the most affected. The uncertainties within months became overwhelming at the peak of pandemic, when they were not only physically at risk but widespread infection brought much more psychological distress, because of expectations the world had from them. Quite a few lost their lives while others struggled to get through. Yet, as the chapters turned, the champions transformed themselves into more resilient and sturdy beings, with mindful leadership and other professionals helping them stay lucid. Governments need to help healthcare organizations, HCWs and their families to overcome financial set-backs, which would take time to stabilize post pandemic. With more insight into the dynamics of the interplay between physical, social, psychological and spiritual factors, we recommend that the efforts and interventions to promote well-being of healthcare workers should continue at local and international level. This will to prevent and limit the long term consequences of the trauma and helping them break the vicious cycle. More researches need to be focused on providing evidence to intervene and promote better mental health outcomes among HCWs as the vaccination produces herd immunity. The frequency and factors associated by anxiety and depression need to be assessed post-pandemic, so that the lessons learnt can be useful for the generations and pandemics to follow.
Although, at present, the battle continues with the 2nd, 3rd and now the 4th wave, but so does optimism, as we continue to believe that, “There was never a night or a problem that could defeat sunrise or hope”.
References
- 1.
Yi W, Tang Y, Yang D, Huang W, Liu H, Sun Z, Yao Y, Zhou Y: Microendoscopic discectomy versus minimally invasive transforaminal lumbar interbody fusion for lumbar spinal stenosis without spondylolisthesis . Medicine 2020,99 (24):e20743. - 2.
Roberti F, Arsenault K: Minimally Invasive Lumbar Decompression and Removal of Symptomatic Heterotopic Bone Formation After Spinal Fusion with Recombinant Human Bone Morphogenetic Protein-2 . World neurosurgery 2020,141 :430-436. - 3.
Amin F, Sharif S, Saeed R, Durrani N, Jilani D: COVID-19 pandemic- knowledge, perception, anxiety and depression among frontline doctors of Pakistan . BMC psychiatry 2020,20 (1):459. - 4.
Otitoloju AA, Okafor IP, Fasona M, Bawa-Allah KA, Isanbor C, Onyeka CS, Folarin OS, Adubi TO, Sogbanmu TO, Ogbeibu AE: COVID-19 pandemic: examining the faces of spatial differences in the morbidity and mortality in sub-Saharan Africa, Europe and USA .medRxiv 2020. - 5.
Bonanad C, Garcia-Blas S, Tarazona-Santabalbina F, Sanchis J, Bertomeu-Gonzalez V, Facila L, Ariza A, Nunez J, Cordero A: The Effect of Age on Mortality in Patients With COVID-19: A Meta-Analysis With 611,583 Subjects . Journal of the American Medical Directors Association 2020,21 (7):915-918. - 6.
Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL: Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers . PloS one 2021,16 (3):e0247679. - 7.
Elhadi M, Msherghi A, Elgzairi M, Alhashimi A, Bouhuwaish A, Biala M, Abuelmeda S, Khel S, Khaled A, Alsoufi A: Psychological status of healthcare workers during the civil war and COVID-19 pandemic: A cross-sectional study . Journal of psychosomatic research 2020,137 :110221. - 8.
Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, Shohaimi S, Daneshkhah A, Eskandari S: The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression . Human resources for health 2020,18 (1):100. - 9.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020 Aug;88:901-907. doi: 10.1016/j.bbi.2020.05.026. - 10.
Tran TV, Nguyen HC, Pham LV, Nguyen MH, Nguyen HC, Ha TH, Phan DT, Dao HK, Nguyen PB, Trinh MV, Do TV. Impacts and interactions of COVID-19 response involvement, health-related behaviours, health literacy on anxiety, depression and health-related quality of life among healthcare workers: a cross-sectional study. BMJ open. 2020 Dec 1;10(12):e041394. - 11.
Trumello C, Bramanti SM, Ballarotto G, Candelori C, Cerniglia L, Cimino S, Crudele M, Lombardi L, Pignataro S, Viceconti ML, Babore A. Psychological adjustment of healthcare workers in italy during the COVID-19 pandemic: Differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between Frontline and Non-Frontline Professionals. International journal of environmental research and public health. 2020 Jan;17(22):8358. - 12.
Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Psychosomatic Research. 2020 Dec 17:110343. - 13.
Cui S, Jiang Y, Shi Q , Zhang L, Kong D, Qian M, Chu J. Impact of COVID-19 on anxiety, stress, and coping styles in nurses in emergency departments and fever Clinics: A cross-sectional survey. Risk Management and Healthcare Policy. 2021;14:585. - 14.
Ahmed H, Allaf M, Elghazaly H. COVID-19 and medical education. The Lancet Infectious Diseases. 2020 Jul 1;20(7):777-8. - 15.
Sharif S, Amin F, Hafiz M, Benzel E, Peev N, Dahlan RH, Enchev Y, Pereira P, Vaishya S, Board WS. COVID 19–Depression and Neurosurgeons. World Neurosurgery. 2020 Aug 1;140:e401-10. - 16.
Sharpe Jr RE, Kuszyk BS, Mossa-Basha M. Special Report of the RSNA COVID-19 Task Force: the short-and long-term financial impact of the COVID-19 pandemic on private radiology practices. Radiology. 2021 Jan;298(1):E11-8. - 17.
Salgado TA, Monteiro GM, Marcon G, Roza TH, Zimerman A, Hoffmann MS, Cao B, Hauck S, Brunoni AR, Passos IC. Loneliness, but not social distancing, is associated with the incidence of suicidal ideation during the COVID-19 outbreak: a longitudinal study. Journal of Affective Disorders. 2021 May 5. - 18.
Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, Sarfraz N, Lee HN, Ghali GE, Liu H, Urman RD. Economic Impact of COVID-19 Pandemic on Health Care Facilities and Systems: International Perspectives. Best Practice & Research Clinical Anaesthesiology. 2020 Nov 17. - 19.
Bandyopadhyay S, Baticulon RE, Kadhum M, Alser M, Ojuka DK, Badereddin Y, Kamath A, Parepalli SA, Brown G, Iharchane S, Gandino S. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ global health. 2020 Dec 1;5(12):e003097. - 20.
Martins RS, Bhatti OA, Mian AI. Violence Against Health Care Workers in Pakistan During the COVID-19 Pandemic. InJAMA Health Forum 2020 Oct 1 (Vol. 1, No. 10, pp. e201263-e201263). American Medical Association. - 21.
Zheng R, Zhou Y, Fu Y, Xiang Q , Cheng F, Chen H, Xu H, Fu L, Wu X, Feng M et al :Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: A cross-sectional study . International journal of nursing studies 2021,114 :103809. - 22.
Devi S. COVID-19 exacerbates violence against health workers. The Lancet. 2020 Sep 5;396(10252):658. - 23.
Sharif S, Amin F, Hafiz M, Benzel E, Peev N, Dahlan RH, Enchev Y, Pereira P, Vaishya S, Board WSCSE: COVID 19–Depression and Neurosurgeons . World Neurosurgery 2020,140 :e401-e410. - 24.
Yurtseven S, Arslan S: Anxiety levels of university hospital nurses during the Covid-19 pandemic . Perspectives in psychiatric care 2021. - 25.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P: Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis . Brain, behavior, and immunity 2020,88 :901-907. - 26.
Tran TV, Nguyen HC, Pham LV, Nguyen MH, Nguyen HC, Ha TH, Phan DT, Dao HK, Nguyen PB, Trinh MV et al :Impacts and interactions of COVID-19 response involvement, health-related behaviours, health literacy on anxiety, depression and health-related quality of life among healthcare workers: a cross-sectional study . BMJ open 2020,10 (12):e041394. - 27.
Trumello C, Bramanti SM, Ballarotto G, Candelori C, Cerniglia L, Cimino S, Crudele M, Lombardi L, Pignataro S, Viceconti ML et al :Psychological Adjustment of Healthcare Workers in Italy during the COVID-19 Pandemic: Differences in Stress, Anxiety, Depression, Burnout, Secondary Trauma, and Compassion Satisfaction between Frontline and Non-Frontline Professionals . International journal of environmental research and public health 2020,17 (22). - 28.
Al Maqbali M, Al Sinani M, Al-Lenjawi B: Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis . J Psychosom Res 2021,141 :110343. - 29.
Cui S, Jiang Y, Shi Q , Zhang L, Kong D, Qian M, Chu J: Impact of COVID-19 on Anxiety, Stress, and Coping Styles in Nurses in Emergency Departments and Fever Clinics: A Cross-Sectional Survey . Risk management and healthcare policy 2021,14 :585-594. - 30.
Ahmed H, Allaf M, Elghazaly H: COVID-19 and medical education . The Lancet Infectious Diseases 2020,20 (7):777-778. - 31.
Sharpe Jr RE, Kuszyk BS, Mossa-Basha M: Special report of the RSNA COVID-19 task force: the short-and long-term financial impact of the COVID-19 pandemic on private radiology practices . Radiology 2021,298 (1):E11-E18. - 32.
Mortier P, Vilagut G, Ferrer M, Serra C, de Dios Molina J, López-Fresneña N, Puig T, Pelayo-Terán JM, Pijoan JI, Emparanza JI: Thirty-day suicidal thoughts and behaviors among hospital workers during the first wave of the Spain COVID-19 outbreak . Depression and anxiety 2020. - 33.
Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, Sarfraz N, Lee HN, Ghali G, Liu H: Economic Impact of COVID-19 Pandemic on Health Care Facilities and Systems: International Perspectives . Best Practice & Research Clinical Anaesthesiology 2020. - 34.
Bandyopadhyay S, Baticulon RE, Kadhum M, Alser M, Ojuka DK, Badereddin Y, Kamath A, Parepalli SA, Brown G, Iharchane S: Infection and mortality of healthcare workers worldwide from COVID-19: a scoping review . BMJ global Health 2020. - 35.
Martins RS, Bhatti OA, Mian AI: Violence Against Health Care Workers in Pakistan During the COVID-19 Pandemic . In:JAMA Health Forum: 2020 : American Medical Association; 2020: e201263-e201263. - 36.
Shahsavari S, Holur P, Tangherlini TR, Roychowdhury V: Conspiracy in the time of corona: Automatic detection of covid-19 conspiracy theories in social media and the news .arXiv preprint arXiv:200413783 2020. - 37.
Devi S: COVID-19 exacerbates violence against health workers . The Lancet 2020,396 (10252):658. - 38.
Organization WH: Coronavirus disease 2019 (COVID-19): situation report, 82 . 2020. - 39.
Cici R, Yilmazel G: Determination of anxiety levels and perspectives on the nursing profession among candidate nurses with relation to the COVID-19 pandemic . Perspectives in psychiatric care 2021,57 (1):358-362. - 40.
Chirico F, Nucera G, Magnavita N: Protecting the mental health of healthcare workers during the COVID-19 emergency . BJPsych International 2021,18 (1). - 41.
CALLING ALL SUPERHEROES: FUNDING THE FIGHT AGAINST COVID-19 . In.: UN foundation; 2020. - 42.
Chow SK, Francis B, Ng YH, Naim N, Beh HC, Ariffin MAA, Yusuf MHM, Lee JW, Sulaiman AH: Religious Coping, Depression and Anxiety among Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective . Healthcare 2021,9 (1). - 43.
Mo Y, Deng L, Zhang L, Lang Q , Pang H, Liao C, Wang N, Tao P, Huang H: Anxiety of Nurses to support Wuhan in fighting against COVID-19 Epidemic and its Correlation With Work Stress and Self-efficacy . Journal of clinical nursing 2021,30 (3-4):397-405. - 44.
Pinho L, Correia T, Sampaio F, Sequeira C, Teixeira L, Lopes M, Fonseca C: The use of mental health promotion strategies by nurses to reduce anxiety, stress, and depression during the COVID-19 outbreak: A prospective cohort study . Environmental research 2021,195 :110828. - 45.
Hofmeyer A, Taylor R: Strategies and resources for nurse leaders to use to lead with empathy and prudence so they understand and address sources of anxiety among nurses practising in the era of COVID-19 . Journal of clinical nursing 2021,30 (1-2):298-305. - 46.
Dincer B, Inangil D: The effect of Emotional Freedom Techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: A randomized controlled trial . Explore 2021,17 (2):109-114. - 47.
Deng Y, Chen Y, Zhang B: Different prevalence trend of depression and anxiety among healthcare workers and general public before and after the peak of COVID-19 occurred in China: A meta-analysis . Asian journal of psychiatry 2021,56 :102547. - 48.
Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, Barrett E, Pal S: COVID-19 Vaccine Acceptance among Health Care Workers in the United States . Vaccines 2021,9 (2). - 49.
Gadoth A, Halbrook M, Martin-Blais R, Gray A, Tobin NH, Ferbas KG, Aldrovandi GM, Rimoin AW: Cross-sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles . Annals of internal medicine 2021. - 50.
Xing K, Tu XY, Liu M, Liang ZW, Chen JN, Li JJ, Jiang LG, Xing FQ , Jiang Y: Efficacy and safety of COVID-19 vaccines: a systematic review .Zhongguo dang dai er ke za zhi = Chinese journal of contemporary pediatrics 2021,23 (3):221-228.