Classification for stiff/ankylosed knees proposed by Sharmal [13].
Abstract
Knee with less than a 50° arc of motion can be considered “stiff.” The surgical exposure in total knee arthroplasty (TKA) is technically challenging in the stiff knees. Other problems like longer operative time, patellar maltracking, rupture or avulsion of patellar tendon, difficulty in flexion-extension gap balancing, bone avulsion, or fracture in the distal femur can occur during TKA. It is not uncommon, and the surgeon needs an extensile surgical approach as early quadriceps release or tibial tubercle osteotomy for adequate exposure. The TKA postoperative outcome is suboptimal with less arc of motion, superficial wound problems, deep infection, and higher late revision surgeries. The rehabilitation protocol should take into account improvements in the range of motion in comparison with the preoperative status, and the patient expectations must be realistic.
Keywords
- total knee arthroplasty
- stiffness
- knee osteoarthritis
1. Introduction
The stiff knee (SKN) is considered as a clinical situation that the range of motion (ROM) is less than a 50° arc of movement [1, 2]. SKN causes a variable level of functional disability, painful discomfort during scarce knee mobility, limp in the gait cycle, and hamper with activities of daily living [3]. Normal walking requires 70°–80° of ROM, stairs require 80°–90° of ROM, and squatting requires at least 130° of ROM [4].
The main causes of SKN are previous surgery on the knee, advanced primary knee ostearthritis, secondary posttraumatic ostearthrosis, reflex sympathetic dystrophy (RSD), neuromuscular disorder, sequelae of previous infection, inflammatory diseases (rheumatoid and psoriatic arthritis), arthrofibrosis, and hemofilic arthropathy. Ankylosis is more common in patients who had their knee immobilized or who are wheelchair bound. The common clinical characteristics in patients with SKN are patela baja, quadriceps contracture, intra-articular adhesions, posterior capsule contracture, poor patellar gliding, and heterotopic ossification [5, 6]. Total knee arthroplasty (TKA) in SKN is a challenging procedure. One of the goals of TKA is to improve knee mobility, including ambulatory ability in the gait [7, 8]. Other goals of TKA in patients with SKN are to relieve pain, improve the alignment to correct the knee deformity, and provide knee stability.
The most relevant factor that predicts knee mobility after TKA is preoperative range of motion [9, 10]. Young age, female sex, and obese patients are more susceptible to achieve less mobility after TKA [11, 12]. In patients with SKNs, the predominant symptom is not mechanical pain. Functional disabilities like impairments in stair climbing, unable to sit on a chair, and inability to walk a long distance are common complaints. Psychological and cosmetic harms are associated with decline in the quality life. TKA is considered a valuable option to improve functional capacity and obtain a mobile knee.
2. Classification
The SKN can be presented clinically in loss of extension (LOE), loss of flexion (LOF), mixed or ankylosed. The major troubles in LOE are adhesions in suprapatellar pouch and in medial and lateral gutters, contracture of extensor mechanism, patellofemoral joint fusion, and loss of tibiofemoral joint space. The SKN in LOF, the extensor mechanism that is elongated with posterior capsule, posterior cruciate ligament (PCL), and collaterals ligaments are contractured. The posterior osteophytes causes a mechanical barrier to achieve complete ROM. Ankylosed knee can be associated with knee arthrodesis, infection, reconstruction after tumor ressection, after severe trauma with distal femur, and tibial plateau fractures. The classification proposed by Sharma [13] is based on the degree of loss of ROM in the knee joint, as shown in Table 1.
|
|
|
|
|
|
Table 1.
This classification provides a guidance for surgeons related to surgical approach, type of prosthetic implants, and helps to presume functional outcome after TKA.
3. Indications
Advanced primary knee osteoarthritis (Kellgren-Lawrence 3 or 4);
Posttraumatic knee osteoarthitis and/or previous knee surgery;
After knee osteotomy (distal femur and/or proximal tibia);
Arthrofibrosis (post-surgery and/or prolonged immobilization);
Inflammatory osteoarthritis (rheumatoid arthritis and psoriasis);
Hemophilic arthropathy;
Ankylosis (after knee arthrodesis);
Heterotopic ossification (HO);
Reflex sympathetic dystrophy (RSD);
Neurologic arthropathy;
Postinfection arthropathy.
4. Contra indications
Neuromuscular disease (s) with RSD;
Paralysis after brain vascular stroke;
Patient inability to follow the postoperative rehabilitation protocol;
Active infection without clinical control.
5. Preoperative evaluation
A through clinical history must include questions about previous conservative treatment and surgeries, period of time that stiffness started, comorbidities, medications, and psychological profile. The physical examination must comprise the preoperative passive and active ROM (flexion and extension), patellar gliding, the amount of flexion contracture, scars, type and flexibility of the angular deformity, gait pattern, and extensor mechanism status (elongated or contractured). Osteoporosis is frequent in SKNs. Complete motor, sensory, and vascular assessment should be performed. Ankle/brachial index and Doppler ultrasound can be useful to estimate the function of blood circulation in the legs.
The imaging exams of the knee should include radiographic evaluation in anteroposterior (AP) and lateral at 30° of flexion (Figures 1 and 2). Special views with maximal and minimal flexion in the sagittal plane should be documented. Long-axis anteroposterior (AP) view can be useful to determine the mechanical and anatomical axis of the lower limbs. The sunrise patellar view at 45° of flexion can demonstrate a severe arthritic involvement, where the patella usually is fused with the anterior femur [2, 5]. A stress view in the coronal plane can be helpful to determine if the angular deformity is rigid or correctable. Presence of hardware is not uncommon in STK patients. Computed tomography (CT) scan may be used to assess bone stock and rule out infections [3].

Figure 1.
Radiography in anteroposterior view with stiff knee.

Figure 2.
Radiography in lateral view with 30° of flexion.
The surgeon must select which type of knee prosthesis will be required. A broad assortment of modular systems are disposable according to each patient. More constrained implants can be considered in cases with bone loss, ligamentous insufficiency, or after extensive soft tissues releases. A custom prosthesis must be fabricated for a particular situation as a very small or large knees and ankylosed knees in rheumatoid patients. In a previous infected STK, a staged procedure can be recommended to decrease the risk of serious complications [14, 15].
6. Surgical technique
The type of anesthesia should emphasize the muscle relaxation and minimize blood loss. Usually, the epidural anesthesia associated with peripheral nerve block as adductor canal provide decrease of narcotic usage and postoperative pain. The tranexamic acid (20–60 mg/kg) can be administrated intravenous during the anesthetic induction in attempt to reduce the blood loss. The use of tourniquet is questionable and can be avoidable in STK patients [16, 17]. The use of sterile drape is recommended, and the leg should be free to move during the TKA. The range of motion (ROM) and ligamentous stability should be addressed prior the incision and documented.
A straight midline incision should be used, if there is not prior surgical scar. If an anterior longitudinal knee scar is found, the skin incision starts more proximally. Usually, the skin is adherent to the subcutaneous tissue and careful dissection may be required to mobilize the skin. This step assists the deep subfascial dissection and facilitates the dermis and epidermis closure. A medial parapatellar arthrotomy is performed with capsule opening and releases the adhesions in the suprapatellar pouch and plane between anterior distal femur underneath the quadriceps tendon. After this step, cleaning the medial and lateral gutters may be required to gain adequate exposure. All the fibrotic tissues should be removed. The patellar tendon is identified and protected during the TKA, and the space posterior to the tendon freed by sharp dissection with the scalpel or eletrocautery.
The next step is the patellar eversion. The difficulty to dislocate the patella laterally, in SKN, remains a problem. The lateral retinacular release can be performed, if the knee remains stiff with flexion less than 40° and the lateral patellofemoral ligament is cut to assist the patellar eversion. An extensive transquadricipital approach, the rectus snip, can be performed to improve and provide good exposure with low risk related to the extensor mechanism damage. The rectus tendon is transected in an oblique fashion, around 45°, in a superior and lateral direction [18]. Orienting the rectus snip distally allows for conversion to a V-Y quadricepsplasty that the surgeon incises the rectus tendon and vastus lateralis, but not the lateral retinaculum [19, 20]. This approach preserves the superior lateral geniculate artery, which provides the major blood supply to the patella, when a medial arthrotomy has been performed. However, this technique is not recommended in the presence of subluxated or dislocated patella laterally. In this scenario, an extensive lateral retinacular release can be performed and the patella is everted and knee is flexed gently. It is recommended to be cautious during this maneuver to avoid patellar tendon avulsion from the tibia tubercle, bone avulsion, and medial collateral ligament (MCL) tear in the progression for the knee flexion [21]. The placement of a metallic pin through the tibial tubercle can decrease the stress over the patellar tendon and hinder the avulsion. The combination of a quadriceps snip and lateral release provides an adequate exposure for most SKNs. The rectus tendon and vastus lateralis muscle are repaired, but the lateral retinacular incision is left open. This approach has the advantage of not requiring modification of postoperative rehabilitation [22].
In the varus deformity, the subperiosteal medial release is then continued, with a sharp scalpel, an electrocautery or an osteotome, as the knee is further flexed and the tibia externally rotated. Dissection should begin in extension on the bone surfaces in attempt to mobilize the soft tissues. Then, skeletonization of the tibia and femur has been performed to allow knee flexion for adequate exposure. For severe varus SKNs, a medial transepicondylar femoral osteotomy may be required. In the valgus deformity with SKNs, a decision must be made to choose an anterior longitudinal traditional incision or lateral approach described by Keblish [23].
The tibial tubercle osteotomy (TTO) can be performed to extend the incision distally for the most difficult SKNs. The osteotomy should encompass at least 8 centimeters (cm) distal to the top of the tibial tubercle. The bone cut is made with an oscillating saw from medial to lateral, and then the lateral cortex is transected with an osteotome. Muscle attachments to the lateral tibial crest with a periosteal soft tissues hinge are left preserved. Two or three wires are passed to encompass the tubercle during closure [24]. Furthermore, two or three screws can be used to stabilize the TTO, in patients with good bone quality. In osteoporotic bone, TTO is not recommended. Before wound closure, the knee was taken through a passive ROM to assure osteotomy fixation and patellofemoral tracking. Postoperatively, the patients wore a protective knee immobilizer while up and walking for the first 6 weeks.
For the ligament balancing, sequential soft tissue release can be performed to correct the angular deformity; if posterior cruciate ligament (PCL) appears to be functional and balanced, cruciate retaining (CR) prosthesis can be used, but this is an uncommon scenario. For a rigid or severe flexion, contracture may be necessary to cut more distal femur (2 mm) to achieve a straight knee in extension. It is not a feasible solution to cut more distal femur than 2 mm due to the high risk to raise the joint line. Then, the tibial and femoral bone cuts are recommended to place the laminar spreaders in extension and flexion in 90°. A curved osteotome is used to remove the posterior osteophytes and release the posterior capsule (Figure 3). This maneuver is essential to open the flexion gap [25](Figures 4 and 5).
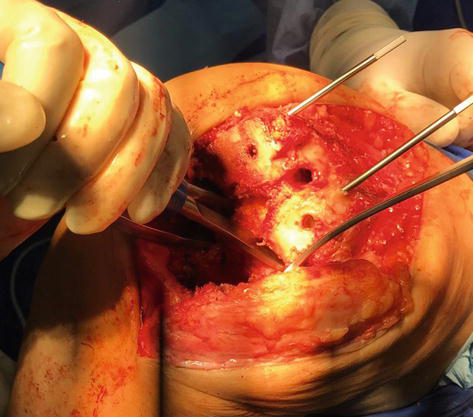
Figure 3.
Removal of posterior osteophytes in the femoral condyles.
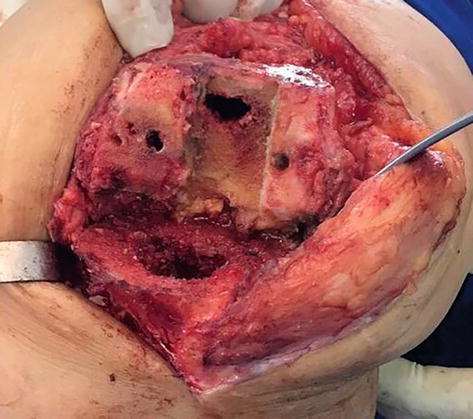
Figure 4.
Narrow flexion gap prior the posterior release.
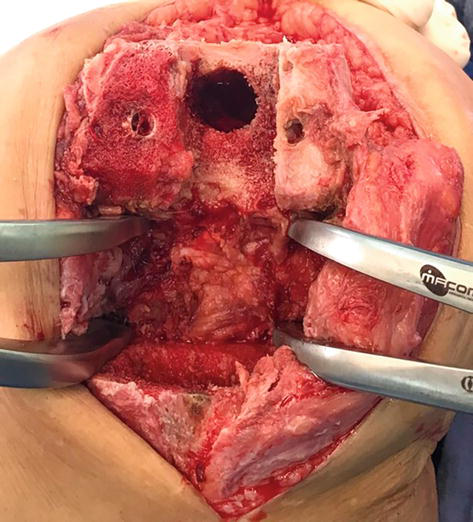
Figure 5.
Opening of the flexion gap with laminar spreaders.
Moreover, more constrained implants as posterior stabilized (PS) models with an elevated polyethylene post are considered as the implant of choice due to the PCL contracture in SKNs. If during insertion of trial components, the knee is unstable in both coronal and sagittal plane, and a more constrained modular component with augments and stems or hinged prosthesis can be chosen. It is recommended to place the femoral component more posterior to decrease the flexion gap, mainly in PS implants. The level of constriction will depend the extent of the ligamentous releases and the amount of bone loss encountered during the TKA. A tumor prosthesis or custom implants may be needed in extremely SKNs, especially in extension. The prosthesis chosen should have options available for femoral and tibial implants in attempt to re-establish the anatomic joint line with available metallic augments (Figures 6 and 7). Care should be taken to avoid overstuff in the patellofemoral articulation that can lead to a flexion contracture and anterior knee pain.

Figure 6.
Postoperative radiography in anteroposterior view after TKA in stiff knee.

Figure 7.
Postoperative radiography in lateral view after TKA in stiff knee.
In ankylosed and after knee arthrodesis, the patellar and proximal tibial cut can be performed in the beginning to obtain more space and promote a better exposure during the TKA. A posterior capsule release with the electrocautery and the laminar spreaders positioned in extension can help after the bone cuts to achieve zero degrees. For a more severe contracture above 30°, the quadricepsplasty may be needed in attempt to elongate the extensor mechanism and to re-establish the joint line. In patients with MCL insufficiency and bone loss in the metaphysis, a hinge TKA can be considered.
The closure of the quadriceps tendon should be performed between 30° and 60° of knee flexion, depending on the preoperative gravity of the SKN. The type of quadriceps release or TTO performed should be taken into account to consider the angulation of knee flexion during the closure. The intraoperative ROM after this surgical step should be documented with a photograph to demonstrate for the patient and the physiotherapist [26].
7. Postoperative management
A light pressure dressing is applied, and cryotherapy can be used to reduce swelling and knee pain. The effectiveness of rehabilitation on functional outcomes depends on the appropriate timing, intensity, and progression of the ROM, accounting for the patient’s ability and level of pain. The use of the removable knee orthosis is debatable. It can be used in static or dynamic manner in attempt to avoid loss of motion after TKA [27]. The patient is immediately placed in a continuous passive motion (CPM) machine from 0° to 30° of flexion in the recovery room. The flexion is increased 10° a day or as tolerated. The physical therapy can be prescribed in the early stage of the postoperative rehabilitation protocol intercalated with the CPM to optimize the gain of knee motion [28]. The pain control is crucial to achieve the progressive ROM. The use of spinal or epidural catheters with analgesic infusion can be helpful after TKA in SKNs. The early quadriceps activation is recommended with physical methods (sensory transcutaneous electrical stimulation), active isometric contraction, and early deambulation with walker or crutches. After TTO and V-Y quadricepsplasty, the rehabilitation protocol is delayed to preserve bone and soft tissue healing, mainly between 4 to 6 weeks. A long orthosis is recommended in the lower limb to keep the gait secure. The recovery of quadriceps function is essential to achieve a satisfactory outcome during the day life activities, improve ROM, and obtain a stable gait [29].
8. Clinical results and complications
The clinical results of TKA in SKNs are inferior in comparison with non-stiff knees with higher complication rates [21, 30]. The rate of complications ranges from 21–35% [31, 32]. The common complications are patellar tendon avulsion, partial or complete tear of MCL, bone fracture or avulsion (epicondyle (s), patella), stiffness after TKA, wound dehiscence, ligamentous imbalance between extension, and flexion gap. Gentle knee flexion and progressive subperiosteal soft tissue releases with the electrocautery can prevent intraoperative bone fracture. It is not uncommon a painful TKA in SKNs that can be a challenging situation to achieve a better functional outcome. Extension lag is associated with V-Y quadricepsplasty [32]. Aseptic loosening in the tibial component has been described in some SKNs [32, 33]. Osteoporotic bone can be considered as a risk factor for fractures around the knee.
The functional scores applied after TKA like Hospital for Special Surgery (HSS), Knee Society Score (KSS), Knee Society Functional Score (FS) have improved due to gain in postoperative ROM in comparison with preoperative status [11, 30, 31, 32, 33]. The range of improvement in ROM after TKA in SKNs is around 50°–70°. The range of improvement in KSS after TKA is between 30 and 45 points [30, 31, 32, 33]. In spite of the enhancement in motion, some residual flexion contracture is predictable in type 2 and 3 SKNs and can affect the pattern of the gait. A limp with overload in the lumbar spine can be expected in this scenario.
The TKA in SKNs is technically demanding with a time-consuming rehabilitation protocol. Patient expectation should be realistic according to the level of SKNs. The complication rate is greater than conventional TKA. A good preoperative evaluation is mandatory to avoid unexpected intra- and postoperative hassle.
References
- 1.
Aglietti P, Windsor RE, Buzzi R, Insall JN. Arthroplasty for the stiff or ankylosed knee. The Journal of Arthroplasty. 1989; 4 (1):1-5 - 2.
Rajgopal A, Ahuja N, Dolai B. Total knee arthroplasty in stiff and ankylosed knees. The Journal of Arthroplasty. 2005; 20 (5):585-590 - 3.
Cuckler JM. The stiff knee: Evaluation and management. Orthopedics. 2002; 25 (9):969-970 - 4.
Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Physics Therapaphy. 1972; 52 (1):34-43 - 5.
Kelly MA, Clarke HD. Stiffness and ankylosis in primary total knee arthroplasty. Clinical Orthopaedics and Related Research. 2003; 416 :68-73 - 6.
Montgomery WH 3rd, Insall JN, Haas SB, Becker MS, Windsor RE. Primary total knee arthroplasty in stiff and ankylosed knees. The American Journal of Knee Surgery. 1998; 11 (1):20-23 - 7.
Lange T, Schmitt J, Kopkow C, Rataj E, Günther KP, Lützner J. What do patients expect from total knee arthroplasty? A Delphi consensus study on patient treatment goals. The Journal of Arthroplasty. 2017; 32 (7):2093-2099 - 8.
Gibon E, Goodman MJ, Goodman SB. Patient satisfaction after total knee arthroplasty: A realistic or imaginary goal? Orthop Clinics. 2017; 48 (4):421-431 - 9.
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty. The Journal of Bone and Joint Surgery. American. 2003; 85A :1278-1285 - 10.
Lizaur A, Marco L, Cebrian R. Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. Journal of Bone and Joint Surgery. British Volume (London). 1997; 79 (4):626-629 - 11.
Gatha NM, Clarke HD, Fuchs R, Scuderi GR, Insall JN. Factors affecting postoperative range of motion after total knee arthroplasty. The Journal of Knee Surgery. 2004; 17 (4):196-202 - 12.
Winemaker M, Rahman WA, Petruccelli D, de Beer J. Preoperative knee stiffness and total knee arthroplasty outcomes. The Journal of Arthroplasty. 2012; 27 (8):1437-1441 - 13.
Sharma M, Sharma S, Upadhyaya AR. Classification-based management of stiff/ankylosed knees. Indian Journal of Orthopology. 2021; 55 (5):1158-1174 - 14.
Bae DK, Yoon KH, Kim HS, Song SJ. Total knee arthroplasty in stiff knees after previous infection. Journal of Bone and Joint Surgery. 2005; 87 (3):333-336 - 15.
Hsu CH, Lin PC, Chen WS, Wang JW. Total knee arthroplasty in patients with stiff knees. The Journal of Arthroplasty. 2012; 27 (2):286-292 - 16.
Liu Y, Si H, Zeng Y, Li M, Xie H, Shen B. More pain and slower functional recovery when a tourniquet is used during total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2020; 28 (6):1842-1860 - 17.
Ahmed I, Chawla A, Underwood M, Price AJ, Metcalfe A, Hutchinson CE, et al. Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery: An abridged version of a Cochrane systematic review and meta-analysis. Bone Joint Journal. 2021; 103 (5):830-839 - 18.
Garvin KL, Scuderi G, Insall JN. Evolution of the quadriceps snip. Clinical Orthopaedics and Related Research. 1995; 321 :131-137 - 19.
Scott RD, Siliski JM. The use of a modified VY quadricepsplasty during total knee replacement to gain exposure and improve flexion in the ankylosed knee. Orthopedics. 1985; 8 (1):45-48 - 20.
Trousdale RT, Hanssen AD, Rand JA, Cahalan TD. VY quadricepsplasty in total knee arthroplasty. Clinical Orthopaedics and Related Research. 1993; 286 :48-55 - 21.
Debette C, Lustig S, Servien E, Lording T, Villa V, Demey G, et al. Total knee arthroplasty of the stiff knee: Three hundred and four cases. International Orthopaedics. 2014; 38 (2):285-289 - 22.
Barrack RL, Smith P, Munn B, Engh G, Rorabeck C. Comparison of surgical approaches in total knee arthroplasty. Clinical Orthopaedics and Related Research. 1998; 356 :16-21 - 23.
Keblish PA. The lateral approach to the valgus knee. Surgical technique and analysis of 53 cases with over two-year follow-up evaluation. Clinical Orthopaedics and Related Research. 1991; 271 :52-62 - 24.
Whiteside LA. Exposure in difficult total knee arthroplasty using tibial tubercle osteotomy. Clinical Orthopaedics and Related Research. 1995; 321 :32-35 - 25.
Fosco M, Filanti M, Amendola L, Savarino LM, Tigani D. Total knee arthroplasty in stiff knee compared with flexible knees. Musculoskeletal Surgery. 2011; 95 (1):7-12 - 26.
Pinsornsak P, Kanitnate S, Boontanapibul K. The effect of immediate post-operative knee range of motion photographs on post-operative range of motion after total knee arthroplasty. International Orthopaedics. 2021; 45 (1):101-107 - 27.
McElroy MJ, Johnson AJ, Zywiel MG, Mont MA. Devices for the prevention and treatment of knee stiffness after total knee arthroplasty. Expert Review of Medical Devices. 2011; 8 (1):57-65 - 28.
Richter M, Trzeciak T, Kaczmarek M. Effect of continuous passive motion on the early recovery outcomes after total knee arthroplasty. International Orthopaedics. 2022; 46 (3):549-553 - 29.
Ha CW, Park YB, Song YS, Kim JH, Park YG. Increased range of motion is important for functional outcome and satisfaction after total knee arthroplasty in Asian patients. The Journal of Arthroplasty. 2016; 31 (6):1199-1203 - 30.
McAuley JP, Harrer MF, Ammeen D, Engh GA. Outcome of knee arthroplasty in patients with poor preoperative range of motion. Clinical Orthopaedics and Related Research. 2002; 404 :203-207 - 31.
Bhan S, Malhotra R, Kiran EK. Comparison of total knee arthroplasty in stiff and ankylosed knees. Clinical Orthopaedics and Related Research. 2006; 451 :87-95 - 32.
Choi YJ, Seo DK, Lee KW, Ra HJ, Kang HW, Kim JK. Results of total knee arthroplasty for painless, stiff knees. Knee Surgery Related Research. 2020; 32 (1):1-7 - 33.
Naranja RJ, Lotke PA, Pagnano MW, Hanssen AD. Total knee arthroplasty in a previously ankylosed or arthrodesed knee. Clinical Orthopaedics and Related Research. 1996; 331 :234-237