Inclusion criteria.
Abstract
One of the most common causes of disability in older adults is osteoarthritis (OA), which often affects the knee. When conventional treatments fail to produce positive changes in patients’ physical function, pain relief, and quality of life, replacement of the degenerated and/or malformed joint is recommended. Total knee arthroplasty (TKA) has been shown to be beneficial in improving aforementioned factors in patients with OA. However, despite comprehensive surgical methods and postoperative rehabilitation approaches, knee extensor weakness persists over a long period of time and may not reach the preoperative level of the non-OA leg for up to 6 months after surgery. Therefore, current rehabilitation programs do not seem to be sufficient to counteract these negative changes after TKA. When overt movement is limited due to various factors, several cognitive strategies have been shown to be useful in improving neuromuscular function without mechanically loading the muscles. One of the most studied strategies is motor imagery (MI). While there is some preliminary evidence supporting the use of MI in TKA rehabilitation practice, an umbrella review with meta-analysis is needed to summarize these findings and draw a clear conclusion about the efficacy of MI in terms of physical function and pain relief in TKA patients.
Keywords
- cognitive practice
- total knee replacement
- pain relief
- physical function
- functional performance
- strength
- range of motion
1. Introduction
Aging is a progressive deterioration at the cellular, tissue and organ levels, resulting in a loss of homeostasis, a reduced ability to adapt to internal and/or external stimuli and an increased susceptibility to disease. Structural changes in various tissues are usually accompanied by negative changes in the functionality of all systems in the human body. With increasing age, there is an increased incidence of various diseases, which further accelerates disability and independence. One of the most frequent occurring causes of disability among older adults is osteoarthritis (OA), which commonly affects a knee due to high mechanical forces stressing the joint. When more conventional, i.e. nonsurgical treatments do not produce positive changes in physical function, pain relief and quality of life, the replacement of the degenerated and/or malformed joint is recommended for OA patients. Depending on the extent of the degenerated tissue, surgical replacement can be either total (e.g., when OA affects both compartments of the knee, TKA) or partial (e.g. when OA is limited to only one compartment of the knee; UKA). However, TKA is preferably performed as surgical treatment in almost 90% of all patients diagnosed with end-stage OA [1]. Since both, the incidence and prevalence of OA increase with age [2, 3], the longer life expectancy that is being faced globally will result in an increase of primary TKA rates which, by the year 2030, are anticipated to grow for more than 6 folds [4].
TKA has been shown as beneficial in improving physical function, pain relief and improving QoL of OA patients. However, despite using comprehensive surgical methods and post-operative rehabilitation approaches, the knee extensors muscle weakness persists over a long period, and might not achieve preoperative levels of the OA unaffected leg for up to 6 months post-surgery [5, 6]. Current rehabilitation practice after TKA consists of a more conventional approach to exercises that mechanically stresses the musculoskeletal system. Such exercise programs include joint mobility exercises to improve range of motion, gait relearning, weight-bearing exercises, neuromuscular function and proprioception training and strength and endurance exercises, using both voluntary and electrically triggered actions [7, 8]. A finding from a recent review and meta-analysis showed that outpatients professionally guided rehabilitation practice group had a consistently lower decline of the OA-affected knee extensors strength in the early periods following TKA when compared to usual care group. However, the authors suggested that strategies focused on preserving neural circuits of motor control must be considered for achieving optimal rehabilitation outcomes.
In the first days after TKA, patients are hardly physically active due to the pain caused by the surgical trauma. Therefore, inpatient rehabilitation is usually performed by passive exercises provided by physical therapists, continuous passive motion devices and transcutaneous electrical stimulation of the lower limb muscles. When overt movement is limited due to various factors (e.g. pain, opioids, cast, etc.), various cognitive strategies have been shown to be beneficial in improving neuromuscular function without mechanically stressing the muscles. One of the most studied strategies is motor imagery (MI). Recently, Paravlic and colleagues published the first systematic review paper with a meta-analysis that examined the effects of mental simulation strategies on physical function in TKA patients [9]. The authors showed a promising result favoring cognitive interventions over routine physical therapy alone, taking into account overall physical function, maximal strength of the affected leg, fast walking speed, timed up-to-go test and active knee joint flexion. Two other reviews were published in last 2 years that examined a similar question [10, 11]. These studies focused exclusively on MI practice only and included several different measures, such as range of motion of the affected knee joint and pain intensity. Currently, there is a substantial body of evidence regarding the effects of MI in the rehabilitation of TKA patients, warranting a collective assessment of their effects in the context of a review and representing a summary effect of MI in this specific patient population.
The purpose of this study was to examine the effects of the MI practice intervention in TKA patients on several measures of physical function and pain intensity using the umbrella review.
2. Methods
This umbrella review with meta-analysis was performed according to guidelines provided by the working group of Aromataris et al. [12], whereas the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) updated statement guidelines were followed [13].
2.1 Search strategy
The main author (AP) performed a literature search on the PubMed, SPORTDiscus and Web of Science online-based databases. The search syntaxes (including keywords) were as follows:
Search: (motor imagery OR mental simulation OR imagery) AND (total knee replacement OR total knee arthroplasty) AND (physical function OR strength OR rehabilitation outcomes) AND (systematic review OR literature review OR meta-analysis).
(((“motor”[All Fields] OR “motor s”[All Fields] OR “motoric”[All Fields] OR “motorically”[All Fields] OR “motorics”[All Fields] OR “motoring”[All Fields] OR “motorisation”[All Fields] OR “motorized”[All Fields] OR “motorization”[All Fields] OR “motorized”[All Fields] OR “motors”[All Fields]) AND (“imageries”[All Fields] OR “imagery, psychotherapy”[MeSH Terms] OR (“imagery”[All Fields] AND “psychotherapy”[All Fields]) OR “psychotherapy imagery”[All Fields] OR “imagery”[All Fields])) OR ((“mental”[All Fields] OR “mentalities”[All Fields] OR “mentality”[All Fields] OR “mentalization”[MeSH Terms] OR “mentalization”[All Fields] OR “mentalizing”[All Fields] OR “mentalize”[All Fields] OR “mentalized”[All Fields] OR “mentally”[All Fields]) AND (“computer simulation”[MeSH Terms] OR (“computer”[All Fields] AND “simulation”[All Fields]) OR “computer simulation”[All Fields] OR “simulation”[All Fields] OR “simul”[All Fields] OR “simulate”[All Fields] OR “simulated”[All Fields] OR “simulates”[All Fields] OR “simulating”[All Fields] OR “simulation s”[All Fields] OR “simulational”[All Fields] OR “simulations”[All Fields] OR “simulative”[All Fields] OR “simulator”[All Fields] OR “simulator s”[All Fields] OR “simulators”[All Fields])) OR (“imageries”[All Fields] OR “imagery, psychotherapy”[MeSH Terms] OR (“imagery”[All Fields] AND “psychotherapy”[All Fields]) OR “psychotherapy imagery”[All Fields] OR “imagery”[All Fields])) AND (“arthroplasty, replacement, knee”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “replacement”[All Fields]) OR “total knee replacement”[All Fields] OR (“arthroplasty, replacement, knee”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “arthroplasty”[All Fields]) OR “total knee arthroplasty”[All Fields])) AND (((“physical examination”[MeSH Terms] OR (“physical”[All Fields] AND “examination”[All Fields]) OR “physical examination”[All Fields] OR “physical”[All Fields] OR “physically”[All Fields] OR “physicals”[All Fields]) AND (“functional”[All Fields] OR “functional s”[All Fields] OR “functionalities”[All Fields] OR “functionality”[All Fields] OR “functionalization”[All Fields] OR “functionalizations”[All Fields] OR “functionalize”[All Fields] OR “functionalized”[All Fields] OR “functionalizes”[All Fields] OR “functionalizing”[All Fields] OR “functionally”[All Fields] OR “functionals”[All Fields] OR “functioned”[All Fields] OR “functioning”[All Fields] OR “functionings”[All Fields] OR “functions”[All Fields] OR “physiology”[MeSH Subheading] OR “physiology”[All Fields] OR “function”[All Fields] OR “physiology”[MeSH Terms])) OR (“strength”[All Fields] OR “strengths”[All Fields]) OR ((“rehabilitant”[All Fields] OR “rehabilitants”[All Fields] OR “rehabilitate”[All Fields] OR “rehabilitated”[All Fields] OR “rehabilitates”[All Fields] OR “rehabilitating”[All Fields] OR “rehabilitation”[MeSH Terms] OR “rehabilitation”[All Fields] OR “rehabilitations”[All Fields] OR “rehabilitative”[All Fields] OR “rehabilitation”[MeSH Subheading] OR “rehabilitation s”[All Fields] OR “rehabilitational”[All Fields] OR “rehabilitator”[All Fields] OR “rehabilitators”[All Fields]) AND (“outcome”[All Fields] OR “outcomes”[All Fields]))) AND (“systematic review”[Publication Type] OR “systematic reviews as topic”[MeSH Terms] OR “systematic review”[All Fields] OR (“review”[Publication Type] OR “review literature as topic”[MeSH Terms] OR “literature review”[All Fields]) OR (“meta analysis”[Publication Type] OR “meta analysis as topic”[MeSH Terms] OR “meta analysis”[All Fields]))
2.2 Translations
Motor: “motor”[All Fields] OR “motor’s”[All Fields] OR “motoric”[All Fields] OR “motorically”[All Fields] OR “motorics”[All Fields] OR “motoring”[All Fields] OR “motorisation”[All Fields] OR “motorized”[All Fields] OR “motorization”[All Fields] OR “motorized”[All Fields] OR “motors”[All Fields].
Imagery: “imageries”[All Fields] OR “imagery, psychotherapy”[MeSH Terms] OR (“imagery”[All Fields] AND “psychotherapy”[All Fields]) OR “psychotherapy imagery”[All Fields] OR “imagery”[All Fields].
Mental: “mental”[All Fields] OR “mentalities”[All Fields] OR “mentality”[All Fields] OR “mentalization”[MeSH Terms] OR “mentalization”[All Fields] OR “mentalizing”[All Fields] OR “mentalize”[All Fields] OR “mentalized”[All Fields] OR “mentally”[All Fields].
Simulation: “computer simulation”[MeSH Terms] OR (“computer”[All Fields] AND “simulation”[All Fields]) OR “computer simulation”[All Fields] OR “simulation”[All Fields] OR “simul”[All Fields] OR “simulate”[All Fields] OR “simulated”[All Fields] OR “simulates”[All Fields] OR “simulating”[All Fields] OR “simulation’s”[All Fields] OR “simulational”[All Fields] OR “simulations”[All Fields] OR “simulative”[All Fields] OR “simulator”[All Fields] OR “simulator’s”[All Fields] OR “simulators”[All Fields].
Imagery: “imageries”[All Fields] OR “imagery, psychotherapy”[MeSH Terms] OR (“imagery”[All Fields] AND “psychotherapy”[All Fields]) OR “psychotherapy imagery”[All Fields] OR “imagery”[All Fields].
Total knee replacement: “arthroplasty, replacement, knee”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “replacement”[All Fields]) OR “total knee replacement”[All Fields].
Total knee arthroplasty: “arthroplasty, replacement, knee”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “arthroplasty”[All Fields]) OR “total knee arthroplasty”[All Fields].
Physical: “physical examination”[MeSH Terms] OR (“physical”[All Fields] AND “examination”[All Fields]) OR “physical examination”[All Fields] OR “physical”[All Fields] OR “physically”[All Fields] OR “physicals”[All Fields].
Function: “functional”[All Fields] OR “functional’s”[All Fields] OR “functionalities”[All Fields] OR “functionality”[All Fields] OR “functionalization”[All Fields] OR “functionalizations”[All Fields] OR “functionalize”[All Fields] OR “functionalized”[All Fields] OR “functionalizes”[All Fields] OR “functionalizing”[All Fields] OR “functionally”[All Fields] OR “functionals”[All Fields] OR “functioned”[All Fields] OR “functioning”[All Fields] OR “functionings”[All Fields] OR “functions”[All Fields] OR “physiology”[Subheading] OR “physiology”[All Fields] OR “function”[All Fields] OR “physiology”[MeSH Terms].
Strength: “strength”[All Fields] OR “strengths”[All Fields].
Rehabilitation: “rehabilitant”[All Fields] OR “rehabilitant’s”[All Fields] OR “rehabilitants”[All Fields] OR “rehabilitate”[All Fields] OR “rehabilitated”[All Fields] OR “rehabilitates”[All Fields] OR “rehabilitating”[All Fields] OR “rehabilitation”[MeSH Terms] OR “rehabilitation”[All Fields] OR “rehabilitations”[All Fields] OR “rehabilitative”[All Fields] OR “rehabilitation”[Subheading] OR “rehabilitation’s”[All Fields] OR “rehabilitational”[All Fields] OR “rehabilitator”[All Fields] OR “rehabilitators”[All Fields].
Outcomes: “outcome”[All Fields] OR “outcomes”[All Fields].
Systematic review: “systematic review”[Publication Type] .or. “systematic reviews as topic”[MeSH Terms] .or. “systematic review”[All Fields].
Literature review: “review”[Publication Type] .or. “review literature as topic”[MeSH Terms] .or. “literature review”[All Fields].
Meta-analysis: “meta-analysis”[Publication Type] .or. “meta-analysis as topic”[MeSH Terms] .or. “meta-analysis”[All Fields] A several additional strategies were used to find any additional reference relevant to this topic as follows:
Google scholar alerts with inception on September 2017;
reading a reference list of the full text articles included
ResearchGate recommendations;
Two online pages i.e. www.elicite.com research assistant and www.connectedpapers.com were utilized, respectively.
Duplicates were identified and removed by two reviewers separately (AP and KD). Two reviewers (AP and KD) independently screened titles and abstracts to identify articles that matched the eligibility criteria.
2.3 Inclusion criteria
The Assessing the Methodological Quality of Systematic Reviews 2 (AMSTAR – 2) rating system was applied to rate and classify all published systematic reviews and meta-analyses into low quality (< 40% items satisfied), moderate quality (40–80% items satisfied) or high quality (>80% items satisfied) [14]. Only systematic reviews with meta-analysis of moderate- and high-quality were included in the present study. Published reviews were included regardless of the original language they were written. There were no restrictions considering a year of publication.
The Participant-Intervention-Comparison-Outcome process for evidence-based practice was followed to describe inclusion criteria Table 1.
| Participants | Male and female patients of all ages who were scheduled for total knee arthroplasty |
| Interventions | For the MI intervention, studies on both visual and kinaesthetic types of imagery and both perspectives of movement representations such as from the first-person view or the third-person view were considered eligible. |
| Comparison group | The effectiveness of MI practice as an independent intervention or in combination with other cognitive interventions was compared to routine physical rehabilitation practice (i.e. physical therapy, exercise intervention) or with placebo intervention if applicable. |
| Outcome | Any measure of physical function such as strength, mobility, balance, self-reported physical function (questionnaires) and pain intensity was considered |
Table 1.
2.4 Methodological quality and quality of evidence evaluation
The main author assessed the methodological quality of the included articles using the AMSTAR – 2 tool. If the assessment was unclear, the consensus was reached by the constructive discussion with a second reviewer (KD). The 16 items of the AMSTAR – 2 checklist were answered with either “yes” or “no”, with each “yes” equaling one point and were classified as mentioned above. In addition, an adapted Grade of Recommendation, Assessment, Development and Evaluation (GRADE) quality of evidence checklist was applied in the included reviews, as it was used previously [15]. The reviews were classified into five GRADE categories: high, moderate, low, very low and no evidence from systematic review. A review was classified as high quality if it contained at least two high-quality studies. Reviews with at least one study of high quality or two studies of moderate quality were classified as moderate quality. If a review contained only primary studies of moderate quality and/or primary studies with inconsistent results, this review was classified as being of low quality. Reviews are classified as of very low quality if they do not contain studies of moderate to high quality. Finally, if the quality of the primary studies was not assessed by the reviewers, the GRADE system was not applied and the review was classified as no evidence from systematic review as recommended previously [15].
2.5 Data extraction
The following data were extracted from the reviews included (a) Study reference; (b) Type of study, number of original studies included, and number of subjects; (c) Objectives of the review; (d) Description of the population; (e) Description of the intervention and comparison group within the review; (f) Number of original studies included in meta-analysis per each outcome measure; (g) Outcome measures; and (h) Main results. Data extraction was performed by the author (AP) and checked for accuracy by a second reviewer (KD).
2.6 Data synthesis and analysis
The meta-analyses were performed using Comprehensive Meta-analysis software (version 3.0). For all reported outcome measures, the standardized mean difference (SMD) along with 95% CIs were calculated. If at least two included studies reported the same outcome and were considered homogenous, then a meta-analysis was conducted and presented with a forest plot. Due to differences in outcomes assessed and measurement scales used between studies, general physical function assessments, self-reported physical function tests and evaluation of the pain intensity were treated separately. Therefore, composite ES (cES) and 95% CI were calculated for each study to overcome the problem of dependence from multiple outcomes and pre-post evaluation periods [16]. A random-effects model of the meta-analysis was used in all comparisons. However, to assess the sensitivity of each meta-analysis conducted, along with random effect, the fixed effect of the meta-analyses was presented. In addition, the publication bias was assessed by examining the asymmetry of the funnel plots using Egger’s test, whereas a significant publication bias was considered if the p value was <0.10. The magnitude of the MI practice effects on outcome measures of interest was interpreted as changes using the following criteria:
3. Results
Figure 1 shows the search strategy process followed for the present review. Initially, NO articles were identified by using predefined search criteria. No additional articles were found by using other sources as mentioned above. Following the initial step, duplicate records were removed and reviews were excluded based on their titles and abstracts. Of this NO of full-text reviews were assessed with only three reviews with meta-analysis were included in this study.
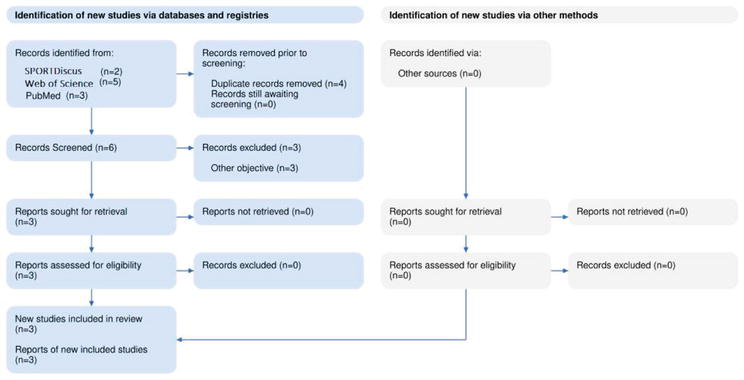
Figure 1.
Flow diagram of included studies.
3.1 Characteristics of the included systematic reviews
The characteristics of the included reviews are presented in Table 2. Current study included 3 systematic reviews with meta-analysis, amounting to 10 original studies (5 overlapping between reviews), 9 RCTs and one non RCT, with a total of 558 participants (Experimental group: 278; Control group: 280 patients). All studies included patients scheduled to total knee arthroplasty, both sexes and aged between 50 and 85 years. In all systematic reviews, the main intervention used MI as adjunct therapy, while two reviews included combination of MI with other cognitive interventions such as action observation and/or guided imagery [9, 11]. Included reviews differed in terms of outcomes assessed. Thus, all reviews assessed affected knee extension strength and timed up to go test. Two reviews assessed pain intensity assessed by Visual Analogue Scale (VAS) [10, 11], while two studies assessed self-perceived knee function [9, 10], and Paravlic et al. [9] self-selected and brisk walking speed under dual and single tasks.
| Study | Data extracted | Description of extracted data |
|---|---|---|
| Paravlic et al. 2020 [9] | Type of study; N°, type of included studies (subjects) | Systematic review and meta-analysis; 7 RCTs, 1 nRCT (n = 228) |
| Objectives | To determine the effectiveness of mental simulation practice (MSP) on measures of physical function recovery in patients who have undergone a joint replacement surgery of lower limbs. | |
| Population | Population: men and women who underwent primary unilateral joint arthroplasty. | |
| Intervention | ||
| N° of studies included in meta-analysis (subjects) per each outcome measure | Physical Function in general, 8 (n = 228); Affected knee extension strength, 2 (n = 46); Uninvolved knee extension strength, 2 (n = 46); Mobility Self-selected gait speed, 4 (n = 153); Self-selected gait speed DT, 2 (n = 47); Brisk walking speed, 2 (n = 47); Brisk walking speed DT, 2 (n = 47); Timed up to go test, 3 (n = 67); Active flexion, 4 (n = 101); Passive flexion, 3 (n = 81); Active knee extension, 2 (n = 57) and Self-reported physical function, 4 (n = 163); | |
| Outcome measures | General physical function; Strength; Mobility; ROM; Self-reported physical function | |
| Results | When compared with standard physical therapy (SPT), MSP showed an effect on physical function in general (effect size [ES], 0.67; 95% confidence interval [CI], 0.38–0.96; nZ7) and maximal voluntary strength of knee extensor muscles of the affected leg (ES, 1.41; 95% CI, 0.64–2.18; nZ2), brisk walking speed (ES, 1.20; 95% CI, 0.58–1.83; nZ2), brisk walking speed with dual task (ES, 1.02; 95% CI, 0.41–1.63; nZ2), timed up-to go test (ES, 0.96; 95% CI, 0.15–1.77; nZ3) and active flexion of the affected leg (ES, 0.70; 95% CI, 0.29–1.11; nZ4). Finally, meta-regression analysis revealed that the effects of MSP were significantly predicted only by the total number of training sessions per study. | |
| Ferrer-Pena et al. 2022 [11] | Type of study; N°, type of included studies (subjects) | Systematic review and meta-analysis; 7 RCTs, (n = 186) |
| Objectives | To assess the impact of MI on strength, active range of motion, pain intensity and physical function in patients with TKA. | |
| Population | Population: men and women who underwent primary unilateral joint arthroplasty. | |
| Intervention | ||
| N° of studies included in meta-analysis (subjects) per each outcome measure | Affected knee extension strength, 4 (n = 104); Active ROM, 6 (n = 152); TUG, 4 (n = 118) and Pain intensity, 5 (n = 132) | |
| Outcome measures | Strength, mobility, ROM and pain | |
| Results | The addition of MI to standard therapy, based on low quality of evidence, showed a moderate increase in quadriceps strength (4 studies; SMD: 0.88; 95% CI: 0.42, 1.34) and a small reduction in pain intensity (SMD: 0.63; 95% CI: 0.08, 1.19). It is unclear whether MI can provide beneficial effects for active ROM and function. | |
| Li et al. 2022 [10] | Type of study; N°, type of included studies (subjects) | Systematic review and meta-analysis; 6 RCTs, (n = 144) |
| Objectives | The study aimed to investigate the effects of motor imagery on the functional performance improvement in patients scheduled for TKA. | |
| Population | Population: men and women who underwent unilateral total knee arthroplasty primarily due to osteoarthritis | |
| Intervention | ||
| N° of studies included in meta-analysis (subjects) per each outcome measure | Affected knee extension strength, 4 (n = 96); TUG, 4 (n = 94) and Self-reported physical function by Oxford Knee Score questionnaire, 2 (n = 46); Pain intensity, 4 (n = 98) | |
| Outcome measures | Strength, mobility, ROM and pain | |
| Results | The MI as adjunct intervention to standard physical therapy showed large effect on strength improvement (SMD = 0.90, 95% CI = [0.47]–[1.32], P < 0.001), reduced pain (SMD = − 0.91; 95% CI = [− 1.29]–[− 0.52], P < 0.001) and improved TUG performance (SMD = − 0.56, 95% CI = [− 0.94]–[− 0.19], P = 0.003) when compared to routine physical therapy alone. However, self-reported physical function by OKS questionnaire, even slightly increased (MD = 0.79-point, 95% CI = [− 0.31]–[1.88], P = 0.159), the observed changes were not significant. |
Table 2.
Summary of reviews with meta-analysis that investigated the effects of motor imagery practice on physical rehabilitation outcomes following total knee arthroplasty (TKA).
3.2 Methodological quality assessment and quality of the evidence evaluation
The methodological quality of the included reviews is presented in Table 3. All three reviews were rated as of high quality using the AMSTAR-2 checklist. Reviews did not provide a list of excluded studies justifying the exclusion reasons (Item 7) and the report of sources of funding of the studies included in the review (Item 10). Only one review [10] did not perform sensitivity analysis considering publication bias (Item 15). The quality of evidence assessed by adopted GRADE principles showed that all three included studies were rated as of high quality.
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | AMSTAR | GRADE |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Paravlic et al. 2020 [9] | YES | YES | YES | YES | YES | YES | NO | YES | YES | NO | YES | YES | YES | YES | YES | YES | HIGH | HIGH |
| Ferrer-Pena et al. 2022 [11] | YES | YES | YES | YES | YES | YES | NO | YES | YES | NO | YES | YES | YES | YES | YES | YES | HIGH | HIGH |
| Li et al. 2022 [10] | YES | YES | YES | YES | YES | YES | NO | YES | YES | NO | YES | YES | YES | YES | NO | YES | HIGH | HIGH |
Table 3.
Overall results of the Assessing the Methodological Quality of Systematic Reviews (AMSTAR-2) and adopted Grade of Recommendation, Assessment, Development and Evaluation (GRADE) quality of evidence checklist.
3.3 Results of meta-analyses
The Egger’s test was performed to provide statistical evidence of funnel plot asymmetry. Results indicated no publication bias for two meta-analyses only: strength (p = 0.139) and TUG (p = 0.225), respectively. For self-reported physical function and pain intensity, a publication bias analysis was not performed, due to low number of included studies.
Nine ESs from three included meta-analyses showed
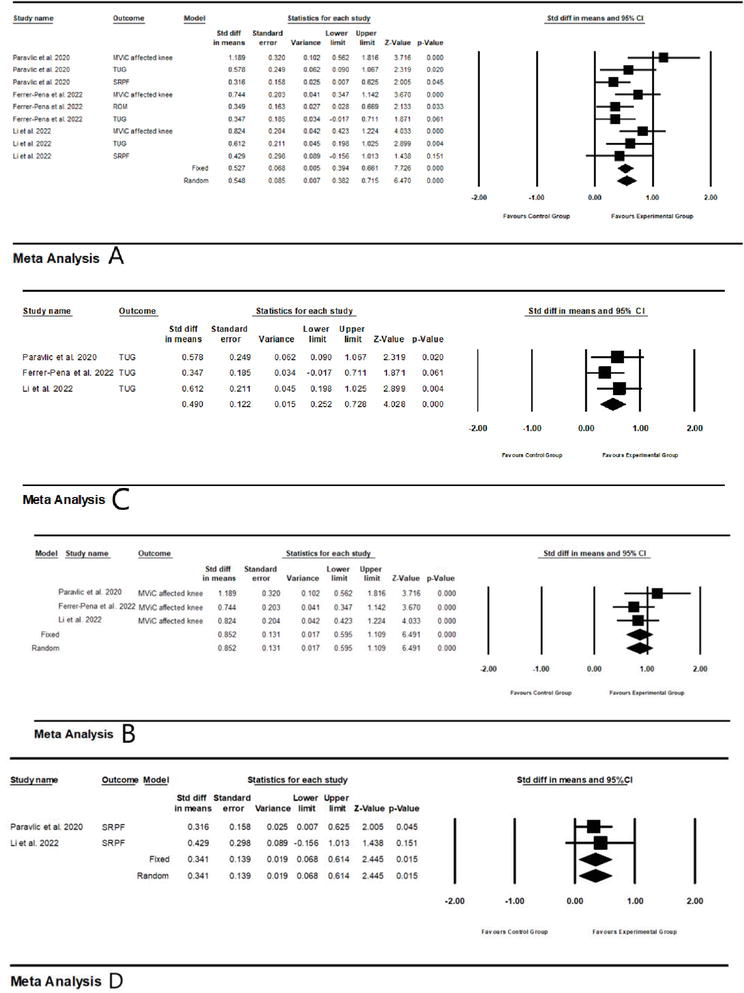
Figure 2.
Summarized effect of MI practice intervention on (A) physical function in general; (B) timed-up to go test; (C) knee extensors strength of the affected knee; and (D) self-reported physical function.
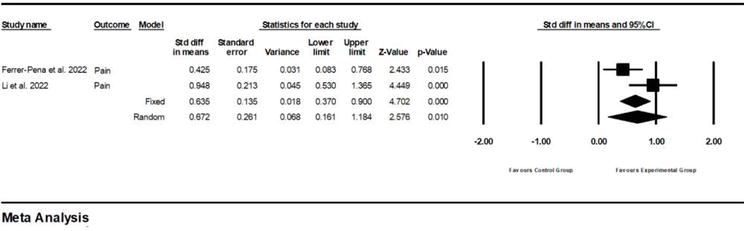
Figure 3.
Effect of MI practice intervention on the pain intensity of the affected knee.
4. Discussion
The aim of this study was to investigate the effectiveness of MI practice as adjunct intervention to routine physical therapy in patients after TKA on measures of physical function and pain.
A current umbrella review with a meta-analysis showed a positive effect of MI on physical function in general (small cES = 0.55), strength (moderate ES = 0.85), timed-up and go test (small ES = 0.49), self-reported physical function (small ES = 0.34), and pain intensity reduction (moderate ES = 0.67) in TKA patients. Given that both fixed and random meta-analysis models showed similar results, these findings can be interpreted as robust.
There are several review articles aimed to investigate the effects of psychological interventions on physical function measures in the apparently healthy [19, 20] and diseased populations [10, 11, 21, 22]. However, these investigations substantially differed in the primary aims, the population included and measures of interests, which consequently resulted in the overall methodology adopted. For example, Paravlic et al. [19] investigated the effects of MI practice on the measures of maximal strength in the healthy adults. Authors found positive effects of MI practice on maximal strength, favoring isometric imagined muscle actions over dynamic muscle actions, whereas a combination of MI with physical practice was found equally effective as physical practice alone [19]. In other reviews, authors investigated the effects of various cognitive strategies in athletes sustaining anterior cruciate injuries (ACL) [21], TKA and total hip arthroplasty patients [9, 22] or TKA patients in isolation [10, 11]. These studies were looking at different measures of interest such as functional mobility [9, 21, 23], balance [9, 10, 11, 23], maximal strength [10, 11, 19] or pain intensity [10, 11] and found equivocal results. Therefore, the current study with a rigorous methodological approach showed robust and positive findings supporting MI practice intervention use in rehabilitation of TKA patients when physical function and pain are primary rehabilitation goals.
Ample evidence suggests that the mechanism underlying effectiveness of imagined contractions relies on both neurophysiological and psychological factors [19, 24, 25]. There is an evidence that imagined movements are functionally equivalent to the physically executed movements in terms of intention, planning, execution duration and task difficulty [25, 26]. The present study found a positive effect of MI on maximal strength and other measures of physical function that are more complex in nature, such as walking and dynamic balance (assessed by TUG test). TUG test is a complex test that evaluates a several motor-related domains such as lower body strength (e.g. getting up from the chair), walking speed (e.g. walking from the chair to the first turning point at a distance of 4.5 m), agility (turning around a cone), and dynamic balance (e.g. all these tasks together). Paravlic et al. showed a positive transfer from simple MI task that focused only on strength to more complex motor tasks mentioned above. The authors also showed that strength improvements following MI practice in TKA patients were significantly and positively correlated with pre-to-post-intervention changes in patients’ kineasthetic (high, r = 0.741) and internal (moderate, r = 0.623) ability to imagine given tasks. This supports previous findings in the literature that the effects of MI depend on the individual’s ability to imagine a particular task as well as the MI type and MI perspective used by the subject [27]. It is suggested that someone who cannot visualize a given task will not benefit from the MI practice [27]. However, Paravlic et al. demonstrated that MI ability can be improved by the MI practice intervention exposure, providing those unfamiliar with MI with new knowledge about how to begin using MI and benefit from it.
In addition to improving physical function, this study showed a positive effect of MI on pain reduction in TKA patients. This finding is consistent with a recent review by Benjamin et al. [28], which showed that MI as adjunctive therapy is superior to standard physical therapy alone in terms of pain reduction and ROM improvements in patients with chronic musculoskeletal conditions. In contrast, the authors found no differences in efficacy between MI and routine therapies acute pain is considered. Because centrally driven mechanisms (e.g. neuroplastic changes and central sensations) [29] predominate in chronic pain, in contrast to acute pain conditions that are driven by peripheral factors (e.g. structural impairment at a peripheral site) [30], the efficacy of MI can be explained by the modulation of cortical areas associated with pain-related cortical reorganization, such as the primary somatosensory cortex, the anterior cingulate cortex and the insula [31]. Although the subsequent mechanisms behind the efficacy of MI in chronic pain are still controversial, MI actually allows activation of motor cortex without overt movement execution [19, 25], sending a motor-related cortical potential via efferents and consequently uncoupling movement from pain perception [28, 31]. Even preliminary data indicate that the MI practice may not be more effective than routine therapy alone, given its mechanism, it could serve to prevent further exacerbation of symptoms and avoid chronic pain events [28].
Considering MI practice programming, only one review with meta-analysis examined a MI practice dose–response relationship, suggesting that effects of cognitive training on outcomes in TKA patients were predicted by the total number of training sessions per study [9]. A recent review by Paravlic suggested recommendations for MI rehabilitation practice in the home setting [32]. In brief, there are some steps that should be followed to benefit from MI practice: (a) patients’ imagery ability must be assessed to inform the therapist which MI perspective and which MI type should be used; (b) it is recommended to provide patients with audio instructions to follow during practice sessions [33]; (c) at the beginning of MI practice therapist should propose simple motor task that is easy to perform by patient and (d) the following motor imagery variables were associated with strength improvement: a training period of 4 weeks, a training frequency of three sessions per week, a training volume of two to three sets, 25 repetitions per set and a single session duration of 15 minutes [19]. While the latter recommendations were compiled from the published literature, the original studies aimed at investigating the effects of different MI practice volumes (training duration, weekly frequency, number of imagined contractions per set, and per single session) are justified.
5. Conclusion
In conclusion, this study provides strong evidence for the use of MI practice as an adjunct to standard rehabilitation treatment in improving physical function and reducing pain after TKA surgery.
Acknowledgments
The author would like to thank the IntechOpen publisher for supporting an open access publication of this article.
Funding
The open access publishing of this article was supported by the Slovenian Research Agency (ARRS) (project no. P5-0147 entitled “The kinesiology of mono-structured, poly-structured and conventional sports,” project manager: Prof. Dr. Matej Supej).
References
- 1.
Campi S, Tibrewal S, Cuthbert R, Tibrewal SB. Unicompartmental knee replacement – Current perspectives. Journal of Clinical Orthopedic Trauma. 2018; 9 (1):17-23 - 2.
Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bulletin of the World Health Organization. 2003; 81 (9):646-656 - 3.
Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis and Cartilage. 2005; 13 (9):769-781 - 4.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. Journal of Bone Joint Surgery. 2007; 89 (4):780-785 - 5.
Paravlic AH, Meulenberg CJ, Drole K. The time course of quadriceps strength recovery after Total knee arthroplasty is influenced by body mass index, sex, and age of patients: Systematic review and meta-analysis. Frontiers in Medicine. 2022; 9 :25 - 6.
Paravlic AH, Kovač S, Pisot R, Marusic U. Neurostructural correlates of strength decrease following total knee arthroplasty: A systematic review of the literature with meta-analysis. Bosnian Journal of Basic Medical Sciences. Feb 5, 2020; 20 (1):1-12 - 7.
Andrade R, Pereira R, Van Cingel R, Staal JB, Espregueira-Mendes J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). British Journal of Sports Medicine. 2020; 54 (9):512-519 - 8.
Kittelson SSK, Stevens-lapsley JE. Neuromuscular electrical stimulation after total joint arthroplasty: A critical review of recent controlled studies. European Journal of Physical and Rehabilitation Medicine. 2013; 49 (6):909-920 - 9.
Paravlic A, Tod D, Milanovic Z. Mental simulation practice has beneficial effects on patients’ physical function following lower limb arthroplasty: A systematic review and Meta-analysis. Archives of Physical and Medical Rehabilitation. 2020; 101 (8):1447-1461 - 10.
Li R, Du J, Yang K, Wang X, Wang W. Effectiveness of motor imagery for improving functional performance after total knee arthroplasty: A systematic review with meta-analysis. Journal of Orthopedic Surgery and Research. 2022; 17 (1):1-12 - 11.
Ferrer-Peña R, Cuenca-Martínez F, Romero-Palau M, Flores-Román LM, Arce-Vázquez P, Varangot-Reille C, et al. Effects of motor imagery on strength, range of motion, physical function, and pain intensity in patients with total knee arthroplasty: A systematic review and meta-analysis. Brazilian Journal of Physical Therapy. Nov-Dec 2021; 25 (6):698-708 - 12.
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. International Journal of Evidence-Based Healthcare. 2015; 13 (3):132-140 - 13.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery. 2021; 88 :1-11 - 14.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017; 358 :1-9 - 15.
Brunner R, Friesenbichler B, Casartelli NC, Bizzini M, Maffiuletti NA, Niedermann K. Effectiveness of multicomponent lower extremity injury prevention programmes in team-sport athletes: An umbrella review. British Journal of Sports Medicine. 2019; 53 (5):282-288 - 16.
Scammacca N. Meta-analysis with complex research designs: Dealing with dependence from multiple measures and multiple group comparisons. Review of Educational Research. 2014; 84 (3):328-364 - 17.
Hopkins MSW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Medicine and Science in Sports and Exercise. 2009; 41 (1):3-13 - 18.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ [British Medical Journal]. 2003; 327 (7414):557-560 - 19.
Paravlic AH, Slimani M, Tod D, Marusic U, Milanovic Z, Pisot R. Effects and dose–response relationships of motor imagery practice on strength development in healthy adult populations: A systematic review and meta-analysis. Sports Medicine. May 2018; 48 (5):1165-1187 - 20.
Tod D, Iredale F, Gill N. “Psyching-Up” and muscular force production. Sports Medicine. 2003; 33 (1):47-58 - 21.
Zach S, Dobersek U, Filho E, Inglis V, Tenenbaum G. A meta-analysis of mental imagery effects on post-injury functional mobility, perceived pain, and self-efficacy. Psychology of Sport and Exercise. 2018; 34 :79-87 - 22.
Bay S, Kuster L, McLean N, Byrnes M, Kuster MS. A systematic review of psychological interventions in total hip and knee arthroplasty. BMC Musculoskeletal Disorders. 2018; 19 (1):1-11 - 23.
Nicholson V, Watts N, Chani Y, Keogh JW. Motor imagery training improves balance and mobility outcomes in older adults: A systematic review. Journal of Physiotheraphy. 2019; 65 (4):200-207 - 24.
Paravlic PR, Marusic U. Specific and general adaptations following motor imagery practice focused on muscle strength in total knee arthroplasty rehabilitation : A randomized controlled trial. PLoS One. 2019; 14 (8):1-19 - 25.
Munzert J, Lorey B, Zentgraf K. Cognitive motor processes: The role of motor imagery in the study of motor representations. Brain Research Reviews. 2009; 60 (2):306-326 - 26.
Jeannerod. The representing brain: Neural correlates of motor intention and imagery. The Behavioral and Brain Sciences. 1994; 17 (2):187-245 - 27.
Martin KA, Moritz SE, Hall CR. Imagery use in sport: A literature review and applied model. Sport Psychologist. 1999; 13 :245-268 - 28.
Yap BW, Lim ECW. The effects of motor imagery on pain and range of motion in musculoskeletal disorders. The Clinical Journal of Pain. 2019; 35 (1):87-99 - 29.
Pelletier R, Higgins J, Bourbonnais D. Is neuroplasticity in the central nervous system the missing link to our understanding of chronic musculoskeletal disorders? BMC Musculoskeletal Disorders. 2015; 16 (1):1-13 - 30.
Mackey S. The “Continuum of Pain” and the American academy of pain medicine. Pain Medicine (United States). 2015; 16 (3):413-415 - 31.
Moseley GL, Flor H. Targeting cortical representations in the treatment of chronic pain: A review. Neurorehabilitation and Neural Repair. 2012; 26 (6):646-652 - 32.
Paravlic AH. Motor imagery and action observation as appropriate strategies for home-based rehabilitation: A Mini-review focusing on improving physical function in Orthopedic patients. Frontiers in Psychology. 2022; 13 (March):1-9 - 33.
Paravlic A, Maffulli N, Kovac S, Pisot R. Home-based motor imagery intervention improves functional performance following total knee arthroplasty in the short term: A randomized controlled trial. Journal of Orthopaedic Surgery and Research. 2020; 15 (1):451